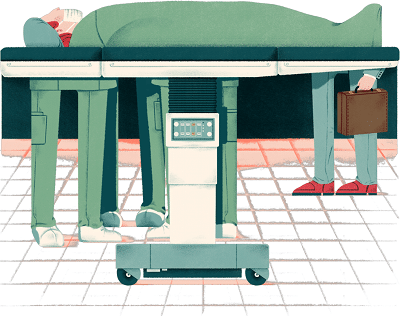
They are a little-known presence in many operating rooms, offering technical expertise to surgeons installing new knees, implanting cardiac defibrillators or performing delicate spine surgery.
Often called device reps — or by the more cumbersome and less transparent moniker “health-care industry representatives” — these salespeople are employed by the companies that make medical devices: Stryker, Johnson & Johnson and Medtronic, to name a few. Their presence in the OR, particularly common in orthopedics and neurosurgery, is part of the equipment packages that hospitals typically buy.
Many “people who don’t work in health care don’t realize that industry reps are sometimes in the OR,” said Josephine Wergin, a risk management analyst for the ECRI Institute, a Pennsylvania nonprofit that conducts research on medical subjects for the health-care industry. “A lot of times they are the real experts on their products.”
Unlike rotating teams of nurses and surgical techs, reps are a consistent presence, experts say, often functioning as uber-assistants to surgeons with whom they cultivate close relationships and upon whom their six-figure salaries depend.
Although they don’t scrub in, reps are expected to be intimately familiar with the equipment they sell, making sure it is at the ready for the surgeon and poised to answer technical questions.
But how much influence do reps wield, how necessary and costly are their services and does their presence in the OR, which may not be disclosed to patients, raise ethical questions about informed consent? A string of court cases has raised questions about their involvement in surgeries that went awry, dating back to the late 1970s when a New York sales manager who had not graduated from high school tried for three hours to fix a prosthetic hip while one of the surgeons is said to have left the OR.
Despite their role, device reps have received little scrutiny, in sharp contrast to drug salespeople, whose role has been the subject of considerable research.
“There’s so little public awareness of this,” said Adriane Fugh-Berman, an associate professor of pharmacology at the Georgetown University School of Medicine and director of PharmedOut, a project that focuses on prescribing and drug-marketing practices. Fugh-Berman is the co-author of a recent study that raises questions about whether surgeons rely too heavily on reps for technical expertise and assistance, to the potential detriment of patients.
But the cost of medical devices, an industry with about $150 billion in annual U.S. sales, combined with concerns about conflicts of interest by doctors who must report industry payments as part of the Affordable Care Act, has resulted in increased scrutiny, as hospitals from Savannah to Stanford seek to standardize and circumscribe the activities of device salespeople.
Several high-profile lawsuits have played a role, among them a 2006 Ohio case in which a surgeon and a rep were ordered to pay a patient $1.75 million after botched brain surgery. The salesperson had wrongly assured the surgeon that a bone cement was suitable for sealing a hole in the patient’s skull.
In 2003, Endovascular Technologies pleaded guilty to 10 felonies in federal court and paid more than $92 million in criminal and civil penalties for covering up problems including 12 deaths associated with an abdominal device. Doctors had been removing the device using a technique devised by reps that had never been approved by the Food and Drug Administration.
Some hospitals, most notably Loma Linda University Medical Center in California, have largely eliminated reps in orthopedics, buying implants directly from the manufacturer at a substantial discount and training surgical technicians to take their place in the OR. Loma Linda’s chief of orthopedics said the hospital has saved about $1 million annually, a savings of about 50 percent on the cost of the devices, without affecting outcomes.
The presence of device reps in the OR, she added, also raises questions about the adequacy of consent, if patients are not explicitly informed of their presence.
ECRI recently repeated its recommendation that hospitals obtain explicit written consent from patients if reps are to be present and warned surgeons against learning “how to use . . . devices on the fly.”
How often that happens is unclear, because what happens in the OR tends to stay in the OR. A small 2014 study suggests that reps’ overinvolvement is not uncommon.
A survey conducted by researchers at New York’s Albany Medical College found that 88 percent of 43 device reps said they had provided verbal instructions to a doctor during surgery, while 37 percent had participated in a surgery in which they felt their involvement was excessive, often because the surgeon lacked sufficient expertise. Twenty-one percent said they had direct physical contact with hospital staff or a patient during an operation, which could violate hospital policy as well as state law.
Terry Chang, associate general counsel of AdvaMed, a device industry trade association, points to its code of ethics as well as newly revised guidelines issued by the American College of Surgeons, which state that reps are to refrain from medical decision-making and participating in surgery.
But Chang says that reps, who have witnessed dozens if not hundreds of the same procedures, provide an essential benefit for doctors and patients. They “are only present at the behest of the physician and only as a trainer,” and they provide “a live interactive resource.”
Their value, Chang said, lies in their expertise, which can make surgery faster and more efficient. “For a lot of institutions, it’s a bandwidth issue,” he said, echoing a finding in Fugh-Berman’s study that some surgeons prefer working with reps because they are more knowledgeable than hospital staff.
Gerald Williams, a Philadelphia joint replacement specialist who is president of the 18,000-member American Academy of Orthopaedic Surgeons, agrees. “Even if a surgeon is extremely familiar” with a device, “there are different teams scrubbing in” who typically have less familiarity with the procedure and the surgeon’s process than a rep with whom a surgeon regularly works.
“Their presence is dictated by the complexity of the surgery,” he said. “They are probably there close to 100 percent in complicated cases such as spine surgery and joint implants.”
Williams said he doesn’t tell his patients that a rep will be in the room, adding, “I don’t tell them there’s a circulating nurse, either. My patients look at me as being the captain of the ship. I think if I told them about a rep, they would all be supportive of it.”
While salespeople have been in operating rooms for decades, their participation mushroomed beginning in the late 1990s with the proliferation of total joint replacement operations, said Linda Groah, the longtime executive director of AORN, the Association of periOperative Registered Nurses.
These days, “there’s much more control of the reps,” she said. “They just don’t come through willy-nilly.’”
But Jeffrey Bedard’s 2014 study about their role in the OR makes it clear that in some cases, there may be a chasm between guidelines and actual practice.
Bedard, who conducted his research as a graduate student in medical ethics, said it was prompted by his experience as an orthopedic device rep in the late 1990s. He subsequently became a drug salesman and now works in the pharmaceutical industry.
Bedard vividly remembers participating in one case involving a patient in her mid-40s. The surgeon, with whom he had not previously worked, refused all preoperative training, including watching a video, on a new $10,000 hip replacement system. “He said, ‘You’re going to be there, right?’ ” Bedard remembers being asked.
“To say that the case was a train wreck would be an understatement,” Bedard recalls. The surgeon repeatedly cursed at him and at the circulating nurse, who continually monitors the patient and is responsible for ensuring that the proper equipment is available, as he struggled to perform the procedure. “I had to hold up the illustrated surgical technique and talk him through the case step by step,” Bedard remembered. “I was absolutely beside myself.”
Bedard recalled that when he called his supervisor to report what had happened, “my boss said: ‘You just made $1,000 for three hours’ worth of work. What are you complaining about?’ ”
Judging by the responses to his anonymous survey, which found that 37 percent of reps said they believed they had been excessively involved in an operation and 40 percent had attended a surgery in which they questioned the surgeon’s competence, Bedard said little appears to have changed. “As a rep,” he said, “you’re paid to sell, to grow your business.”
Two years ago, Gary Botimer, a joint replacement specialist who is chief of orthopedics at Loma Linda, undertook a radical experiment: He got rid of reps in joint replacement cases. Botimer negotiated a steep discount on the price of artificial joints bought in bulk from a well-known American manufacturer and sent hospital surgical techs to the technical training given to device salespeople.
“It took me two years to convince the administration” to do this, recalled Botimer, who said that one surgeon, who had significant financial ties to a manufacturer, quit. “I took a lot of bullets.”
“What we basically did is to take the skill set of the reps and replace it with our own employees, who don’t have a conflict of interest,” Botimer said. “It’s very easy to train your own people. We have found that the techs are better than the reps.”
To lay the groundwork, Botimer said he and other surgeons reviewed the literature to select the best implants as the hospital’s standard. After the program was launched in 2014, Botimer said, he and his staff tracked the outcomes of all 500 joint replacement cases for one year to see if the “rep-less model” was equivalent. No difference in outcomes was detected, he said, but the hospital saved $1 million each year. (While standard implants are used in about 90 percent of cases, Loma Linda surgeons are free to use other devices if they believe doing so is in the patient’s best interest.)
The program has been so successful that it is being extended to other orthopedic surgeries, such as trauma and spine operations, he said. Botimer added that he is fielding inquiries from other hospital systems contemplating a similar move.
“This is a big change in the culture, and no one makes that change easily,” he said. “You have operating [room] personnel who’ve only known one way of doing things, doctors who are afraid to try it and administrators worried that docs would turn on them. We’ve spent a couple of years proving to everybody that their worst fears didn’t happen.”
— Kaiser Health News By Sandra G. Boodman